Diabetic Retinopathy
What is diabetic retinopathy?
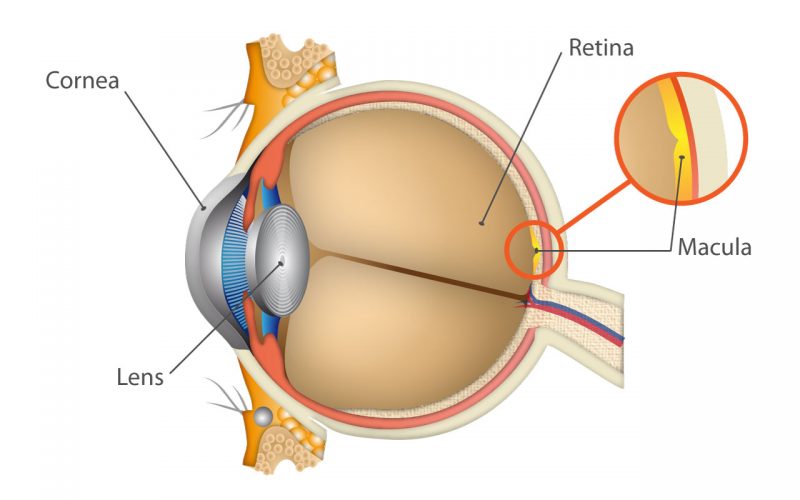
Diabetic retinopathy is a disease that results from diabetes. It can damage blood vessels inside the retina and result in vision loss. The disease usually affects both eyes. Any patient with type 1 or type 2 diabetes is at risk. There are two types of diabetic retinopathy: nonproliferative (or background) and proliferative. Many diabetics have the milder nonproliferative type that usually does not affect vision. The proliferative type is more severe and occurs when new blood vessels grow on the surface of the retina. It often results in the sudden onset of floaters when the abnormal vessels bleed into the vitreous cavity of the eye.
What causes diabetic retinopathy?
Diabetes, which produces high blood sugar levels in the body, can damage the blood vessels in the retina. At the most advanced stage of diabetic retinopathy, new blood vessels may develop. These blood vessels are fragile and easily bleed. This condition may result in severe vision loss or even blindness.
A condition called macular edema can also cause visual loss in patients who are diabetic. The eye’s macula, which provides central vision and allows one to see fine details, can become swollen when fluid leaks into it. This results in blurred vision.
Can diabetic retinopathy be treated?
The good news is that early detection and advancements in treatments can help reduce vision loss caused by diabetes. There are different treatments for different conditions. Nonproliferative diabetic retinopathy is managed by decreasing a patient’s blood sugar levels. The laser procedure for proliferative retinopathy, called pan-retinal or scatter laser, shrinks the newly formed abnormal blood vessels. Multiple laser treatments may be required.
Diabetic macular edema is treated by laser, Avastin® or steroid injections. For patients experiencing an excessive amount of bleeding in the vitreous cavity, a procedure is performed that removes the vitreous gel clouded by the blood and replaces it with a salt solution.
The key to preventing vision loss is early detection. People with diabetes should see an ophthalmologist at least once a year, especially if any change in vision, such as blurred vision or a sudden increase in floaters, is detected.

 New technology, however, is available to help monitor your Dry AMD from home that can catch the progression from Dry to Wet AMD as early as possible, which allows your doctor to begin treatment sooner to help preserve your functional vision. The ForeseeHome® AMD Monitoring Program is a simple, FDA-cleared, at-home daily test that monitors for tiny changes in your vision. Test results are automatically sent from the device to Notal Vision (the makers of ForeseeHome), who alert us of any significant changes in a patients’ vision so we can schedule a follow up appointment and decide on the best course of action.
New technology, however, is available to help monitor your Dry AMD from home that can catch the progression from Dry to Wet AMD as early as possible, which allows your doctor to begin treatment sooner to help preserve your functional vision. The ForeseeHome® AMD Monitoring Program is a simple, FDA-cleared, at-home daily test that monitors for tiny changes in your vision. Test results are automatically sent from the device to Notal Vision (the makers of ForeseeHome), who alert us of any significant changes in a patients’ vision so we can schedule a follow up appointment and decide on the best course of action.